This past weekend, IWK Health put its emergency preparedness to the test with a large-scale simulation of a Code Orange response, a hospital-wide protocol for managing mass casualty events. The exercise brought together over 300 participants, including staff, physicians, learners, community partners, and volunteers, all working together to ensure we’re ready should the unthinkable happen.
It’s the first time since 2018 that IWK has run a disaster simulation of this size and scope, and notably, it was the first to involve all levels of staff, from frontline care providers to the CEO and Board of Directors, as well as many departments across the organization. This marks a major milestone in strengthening our collective preparedness and response capabilities.
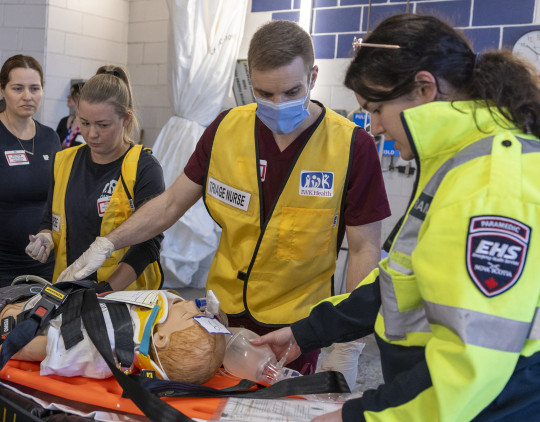
The simulation scenario was designed to mimic an external mass-casualty event and spanned many key areas of the hospital, including the Emergency Department, Pharmacy, Lab, Perioperative Services, PICU, and the Emergency Operations Centre. Participants included doctors, nurses, ward clerks, triage nurses, pharmacists, respiratory therapists, child life specialists, and many more, all playing a vital role.
In addition to caring for the physical needs of our patients, the simulation also tests our psychosocial support plan. This involved setting up and operating a Family Information Support Centre (FISC) to assist in the reunification of families seeking missing loved ones and the Psychological First Aid Centre (PFAC) to provide psychological first aid, immediate support and follow-up support outside the hospital.
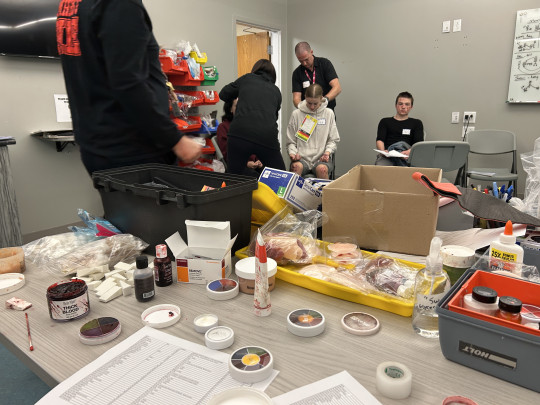
The weekend exercise was months in the making, led by Vered Gazit, medical director of Emergency Preparedness and pediatric emergency physician and Phil Porter, consultant for Emergency Preparedness. Behind the scenes, teams worked tirelessly to ensure every detail was as authentic as possible, right down to the makeup and prosthetics for “injured patients”.
The Red Team, made up of about 140 healthcare and support staff, was responsible for delivering care and support to patients and families. In contrast, the Dark Team of 90 evaluators, simulation specialists, and support personnel closely observed every detail of the exercise. Evaluators were assigned to each care zone to assess not just the clinical response, but also how teams managed the intense emotions, uncertainty, and logistical challenges that come with a mass casualty event.
Adding to the realism, around 70 children, parents, and community members volunteered as simulated patients and family members. Their dedication, portraying scared and distressed parents, upset and confused youth, and patients in varying states of emergency, helped create a dynamic, immersive environment. Each simulated patient had a parent or “shadow” who followed them through their journey, offering valuable feedback on the experience during the debrief session.
The simulation also included challenging scenarios such as intrusive media reporters and waves of casualties, allowing staff to navigate not only medical care but also the communication and coordination challenges that arise in real disasters.

This exercise served as a catalyst to improve both hospital-wide and departmental emergency preparedness plans. Importantly, it also highlighted collaboration with external partners like EHS and QEII, ensuring effective coordination in the event of a real disaster.
As a result of this training, emergency preparedness specialists from Nova Scotia Health attended to observe and learn from IWK’s model, and OPOR has since adopted IWK’s disaster rapid registration system as the new provincial standard, an incredible testament to the expertise and innovation demonstrated by the team.
The post-simulation debrief offered valuable insights into what worked well and where improvements are needed, identifying bottlenecks, critical areas for attention, and practical changes to strengthen IWK’s emergency preparedness going forward.
Thank you to everyone who participated and supported this crucial initiative.