Prolonged and repeated use of antibiotics in children with leukemia and lymphoma can create an environment that favors pathogenic bacteria and antibiotic resistance genes, says recent research out of the IWK. The study shows repeated courses and longer durations of antibiotics commonly given during periods of fever was associated with an increase in ‘bad’ bacteria and a decrease in ‘good’ bacteria in the microbiome. It may also increase antibiotic resistance genes in gut bacterial community.
Published in Frontiers in Cellular and Infection Microbiology The gastrointestinal antibiotic resistome in pediatric leukemia and lymphoma patients indicates the need for protocols to make sure antibiotics are used appropriately and not indiscriminately.
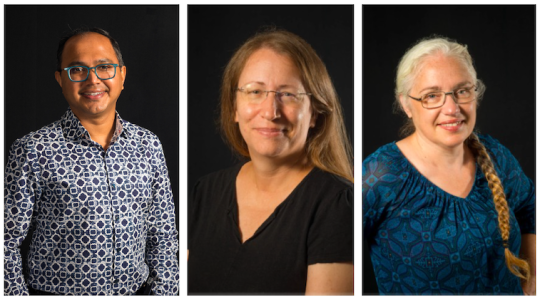
“Patients with cancer are at very high risk of infections,” says IWK hematologist, oncologist and principal investigator Dr. Ketan Kulkarni. “Any fever in cancer patients is considered a medical emergency and must be treated immediately. Very often it means one or more intravenous (IV) antibiotic.”
“Our research focused on the effect of antibiotics on the “resistome” or antibiotic resistance genes found in bacteria in the microbiome of the gastrointestinal tract,” says IWK Clinical Pharmacy Specialist Dr. Tamara MacDonald. “We found that children with leukemia/lymphoma who received repeated courses of antibiotics resulted in increases in the abundance of the bacteria that can harbor these antibiotic resistant pathways.”
Researchers studied stool samples of patients to see whether they contained antibiotic resistance genes. They found multidrug efflux pump genes (proteins that allow microorganisms to regulate their internal environment by removing toxic substances, including antimicrobial agents) and genes that regulate them. Their presence can result in resistance as they identify antibiotics as toxic and pump them out. This could potentially allow opportunistic pathogens to persist and increase even with the use of antibiotics.
These genes also enhance the ability of these pathogens to survive in stressful environments, like those created during oncology treatment. This could also contribute to increases in opportunistic pathogens in the gastrointestinal tract, which is problematic as the gastrointestinal tract is weakened during treatment and there is an increased likelihood of bacteria entering the blood stream and causing life-threatening infections.
“Most genes that are responsible for resistance perform other functions and it is mutated forms of the genes or the acquirement of these genes by other bacteria that leads to resistance,” says Dr. Katherine Dunn, research associate with Dr Kulkarni’s team. “Just because we find antibiotic resistance genes doesn’t mean resistant bacteria are present. The presence of these genes in the microbial community though does signal the potential for resistance and monitoring especially in this vulnerable population is valuable.”
“This research shows that we need to be more vigilant regarding the use of antibiotics in this population,” says MacDonald. “And only use when required and for as little amount of time as required to try to reduce the emergence of devastating resistant pathogens. We need to constantly revise our protocols to optimise them”
“Antibiotics use and abuse is a global problem,” says Kulkarni. “All of us need to collectively remember to use antibiotics appropriately to handle this global problem. Indiscriminate and inappropriate use can lead to a major challenge with resistance.”
This research was funded by the Nova Scotia Health Research Foundation (now Research Nova Scotia), the Beatrice Hunter Cancer Research Institute and through the support of the IWK Foundation, through the JD Irving Fund and an IWK Project Grant.